Experts Speak Out
Sharps safety has fallen off the radar and there is a complacency to the extent that there will probably be a resurgence in injuries simply because there is no one to strongly advocate [for better technology].
—Mary Foley, RN, MS, PhD, past president, American Nurses Association, Nov. 2010
We know too many health care professionals are still at risk of a sharps injury and that more work needs to be done.
—Karen A. Daley, PhD, MPH, RN, FAAN - President, American Nurses Associantion, Nov. 2010
By GENE O’CONNELL – RN, MS
Past Chair of National Association of Public Hospitals and Health Systems
Past CEO of San Francisco General Hospital.
An open letter to:
Congressman Frank Pallone
Healthcare Sub-Committee Chair
2125 Rayburn House Office Building
Washington, D.C., 20515
Dear Congressman Pallone,
I commend Senator Waxman’s Sub-committee hearings on Medical Devices on June 18, 2009 as a critical component of healthcare reform to bring before Congress issues of regulatory oversight to ensure safe, cost effective medical devices that provide better healthcare.
Nowhere in the transcript of testimonies by the four prominent witnesses on June 18, 2009 was there mention of the historic U.S. Needlestick Safety and Prevention Act 2000. Internationally, this uniquely American legislation is the foundation for parliamentary discussions of healthcare reform around the world. The Needlestick Safety and Prevention Act is held as the highest standard of humanistic and wisdom-filled governance to ensure patient and healthcare safety.
Furthermore, the Act addresses the enormous hidden costs of needlestick injuries to society. Dr. William Maisel stated the case succinctly that healthcare reform in America would improve if we only implement current laws.1
In the words of Elise Beltrami, medical epidemiologist at Contamination Disease Control, the CDC’s goal is to completely eliminate needlesticks. “We don’t give a time frame for doing that, and clearly it’s going to be a challenge. But with education, training, appropriate device development and implementation, and developing a culture of safety, it’s a potentially realistic goal.”2 CDC’s national objective can only be achieved by fully supporting the U.S. Needlestick Safety & Prevention Act. The Act is groundbreaking and requires the involvement of frontline healthcare workers in the evaluation, selection and implementation of safer needle devices in particular during the routine blood draw.
In 2000, the Act specifically named the then existing ways to improve safety needles: blunting, sheathing, or retracting the needle for injection equipment (syringes,), IV access devices, lancets, and phlebotomy needles. The U.S. Needlestick Safety & Prevention Act proscribes that U.S. manufacturers offer the safest devices available, and acknowledged that in the future better devices would be invented:
In addition to the existing requirements concerning exposure control plans, the review and update of such plans shall be required to also–
(A) ‘Reflect changes in technology that eliminate or reduce exposure to bloodborne pathogens’; and
(B) ‘Document consideration and implementation of appropriate commercially available and effective safer medical devices designed to eliminate or minimize occupational exposure’. (29 CFR 1910.1030(c)(1)(iv)
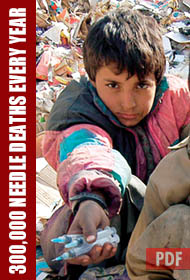
Since the Act became effective and amended the OSHA Bloodborne Pathogens Standard, dozens of new device technologies are used daily across America, improving safety to both healthcare workers and patients, notably in reducing needlestick injuries and contamination. But we’re not out of the woods, as still hundreds of thousands of U.S. healthcare workers continue to receive accidental needlesticks annually.
I am not endorsing these products or companies, but by way of example, since 2000 market leaders, Greiner Bio-One and Becton-Dickinson, have introduced blood collection needles that inform the phlebotomist of needle placement before insertion of the vacuum tube, the current worldwide standard device used 3 billion times annually.3 These are medical breakthroughs, like other new technologies including soft tubing in the IV set, (reduces the potentially dangerous memory of the collection tubing), and medicine injection technologies with safety components that provide the safety of vein entry indication passively and without major additional cost to the procedure.
These safety devices represent issues that are responsible for tremendous hidden costs to our healthcare system. For example, in the U.S. alone, every year hundreds of thousands of healthcare workers are exposed to deadly viruses as a result of needlestick and sharps injuries, and before they can return to work, they must test to rule out HIV and Hepatitis at cost of $3,000 – $5,000 for each person,4 effectively costing hundreds of millions of dollars annually simply for testing due to the needlestick technology. Amber Hogan, MPH Manager, Health Affairs, Becton Dickinson, summed up the costs to society: “The real and immediate risk of exposure to healthcare facilities include days away from work, medical evaluation and follow up, counseling, emotional distress, side effects from drug prophylaxis, decrease staffing and workers’ compensation costs, to name a few.”
Please use America’s current interest in healthcare reform to shine a spotlight on the Needlestick Safety and Prevention Act 2000. OSHA should review the Act as part of the current healthcare reform legislation, and regarding the new safety devices now available, OSHA should be directed to amend its regulations to include the new available technologies. This is supporting standing U.S. law, and exactly in congruence with the fine testimony given to Congressman Waxman’s Sub-committee on Medical Devices.
I am the former chair of the National Association of Public Hospitals and Health Systems, and was the CEO of San Francisco General Hospital and Trauma Center for over a decade before retiring in March of this year. San Francisco General is one of the nation’s top tertiary academic medical centers and safety net institutions, and has received numerous national awards including the 2008 American Medical Association Ethical Force Programs Awards for its patient centered communications initiative as well as recognition for many advances in emergency care and HIV treatment and research.
It is in everyone’s best interest that our current healthcare reform insures that the United States has the most up-to-date and innovative technology that fully supports patient and health care worker’s safety. We must not let the gains of this historic legislation fall by the way side in our rush for health care reform. I urge you to include in your deliberations on medical device regulation the need to support the Needlestick Safety and Prevention Act towards continued oversight in safety, cost-effectiveness and quality control of all medical devices. Without such discussion, healthcare reform will have missed a valuable opportunity, and in so doing perhaps lead to the evisceration of the Act’s effectiveness.
Please enter this letter into the post-record of the June 18, 2009 hearings following Sub-committee discussions. I request that you keep me abreast of your receipt of this correspondence and further discussion how new legislation will support the U.S. Needlestick Safety and Prevention Act 2000.
Sincerely,
Gene Marie O’Connell, RN, MS
REFERENCES
1 Marcia Crosse, Government Accountability Office, William H. Maisel, M.D. M.P.H, Director Medical Device Safety Institute, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, Phillip J. Phillips, Independent Consultant, Peter Lurie, M.D., M.P.H. Deputy Director, Health Research Group.
2 General Accounting Office (GAO) 2000 Occupational Safety: Selected Cost and Benefit Implications of Needlestick Prevention Devices for Hospitals, GAO-01-60R. www.gao.gov/new.items/d0160r.pdf
3 See attached product literature from Greiner Bio-One and Becton Dickinson.
4 Wilburn, MPH, RN., Susan Q. “Needlestick and Sharps Injury Prevention”, Online Journal of Issues in Nursing, September 30, 2004.